By PATRICIA JONES
and DR. MIRANDA CURTISS
With President Trump testing positive for COVID-19 last week and Box Butte County experiencing our first COVID-related death, it is time to revisit the discussion about wearing masks.
Last week during the Chamber’s political forum at the Alliance High School Performing Arts Center several questions were submitted regarding the school’s COVID policies, specifically regarding the number of students being quarantined and the Board’s decision to make the wearing of masks optional.
After the forum, I was contacted by Dr. Miranda Curtiss, AHS class of 99. Dr. Curtiss completed medical school and earned a Ph.D. in Immunology at the University of Iowa. She has completed further fellowships in Pulmonary Medicine and Allergy/Clinical Immunology, and is currently a staff physician at the University of Alabama Birmingham Hospital. She also works in a lab that performs basic research on COVID-19. Dr. Curtiss was especially concerned about the attitude that COVID wasn’t that serious and that we didn’t really need to follow the directed health measures, particularly that so many in Alliance did not see the need to wear masks.
COVID has taken a high toll on the people of Alabama, with 159,169 cases and 2,556 deaths. 12,202 cases have occurred among healthcare workers. Like Nebraska, Alabama has cities and rural areas. Like Nebraska, Alabama has seen some rural areas develop and sustain high COVID-19 infection rates. She urges Nebraskans to look to other states and learn from the lessons and life lost there to avert a similar crisis here. Nebraska is now a red state, which means we have more than 25 new cases per 100,000 people daily.
WHAT ARE THE RISKS?
Even with wearing appropriate Personal Protective Equipment (PPE), health care workers are 3.5 times more likely to contract COVID than the general population. Curtiss wanted to stress that school staff are also at an elevated risk. So are first responders (policemen, firemen) and those working in essential jobs, including healthcare, childcare, schools, agriculture, energy, waste, trades, and critical retail (grocery stores, mechanics, hardware stores, etc.). Wearing a mask protects these essential workers so they can continue to do their jobs.
About 40-45% of COVID-19 infectious children are asymptomatic. However, these asymptomatic infections still spread the disease! An exposed at-risk family member (due to age or medical problems) could easily develop a severe, life-threatening infection.
Symptoms may appear 2-14 days after exposure to the virus, and people are contagious before symptoms occur. Major symptoms of COVID-19 are a new loss of taste or smell, new cough, or shortness of breath and difficulty breathing. Other symptoms, which are common to several diseases and seasonal allergies include fever or chills, fatigue, muscle or body aches, headache, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. Severe symptoms require a visit to the hospital emergency room or a call for an ambulance: trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, bluish lips or face.
Long-term effects of COVID-19 infection have been identified, even in young adults or those with mild or asymptomatic infections. These include chronic cough, fatigue, joint pain, shortness of breath, and headache. It obviously infects the lungs but some individuals will go on to develop lung scarring that requires chronic oxygen therapy. It can affect the heart causing inflammation of the heart muscle (myocarditis) or the sac around the heart (pericarditis) which can cause chronic shortness of breath, chest pain and arrhythmias. It can also affect the brain and kidneys, causing strokes, neurologic disease, and may cause kidney disease severe enough to shut down the kidneys and require dialysis. This is not just theoretical; doctors everywhere around the country are seeing this happen in front of them.
About 5% of COVID-19 cases are severe. Risk factors for severe COVID include age over 60, obesity, diabetes, COPD, cancer, cardiovascular disease, chronic kidney disease, and male gender. Even in people with well-controlled diseases. There are an additional 12 medical diseases on the CDC website that might increase risk of severe COVID but have less clear-cut evidence.
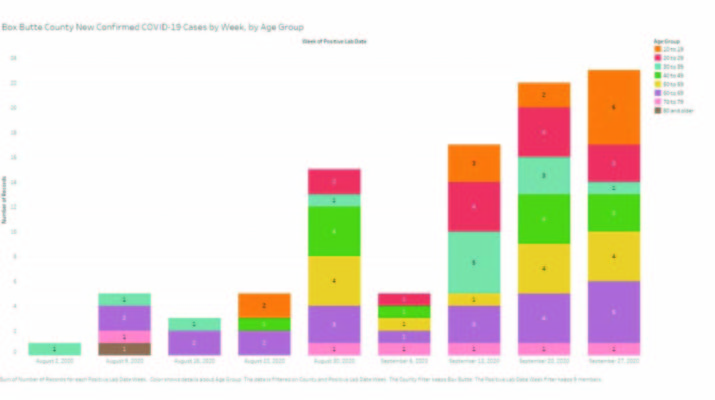
The time to act in Box Butte county is today, right now. Test positivity rates in the Panhandle have risen to 15%, the highest to date in the region. COVID-19 is spreading in the community. The Panhandle Public Health COVID-19 dashboard shows that community spread of COVID is higher in Box Butte and Dawes counties than in surrounding counties. For reference, in 2018 Box Butte County had about 2,900 residents estimated to be over 60 years old (20% of the 11,100 residents in the county). In Nebraska the obesity rates are 12-15% of children and teens (27% of the Box Butte County population) and 34% in the general population (predicting about 3100 people in Box Butte county are obese). Diabetes rates in Nebraska are roughly 10% of the population. You can see how quickly this adds up. There are thousands of people in Box Butte County at risk of severe COVID-19 at all ages, but particularly the elderly.
WHY WEAR MASKS?
The CDC recommends that you wear a cloth face mask when you’re around people who don’t live with you and in public settings when social distancing is difficult. In other words, if you are inside a building and someone else is or has been in the same room, you should probably be wearing a mask IN ADDITION to keeping 6 feet away from anyone else.
A cloth mask or disposable paper mask is intended to trap droplets that are released when the wearer talks, coughs or sneezes. Asking everyone to wear cloth masks can help reduce the spread of the virus by people who have COVID-19 but don’t realize it.
The best protection from the spread of disease is to trap droplets from the person wearing the mask so those droplets don’t infect others. There is also evidence that the use of masks can reduce the number of infectious particles that an exposed individual breathes in; therefore that individual is more likely to have a mild infection rather than a severe infection.
Cloth and paper face coverings are most likely to reduce the spread of the COVID-19 virus when they are widely used by people in public settings. Countries and states that required face masks, testing, isolation and social distancing early in the pandemic have successfully slowed the spread of the virus.
While surgical and N95 masks may be in short supply and should be reserved for health care providers, cloth face coverings and masks are easy to find or make, and can be washed and reused. Masks can be made from common materials, such as sheets made of tightly woven cotton. Instructions are easy to find online. The CDC website even includes directions for no-sew masks made from bandannas and T-shirts.
COVID-19 will always be with us. Eventually we will have vaccines. We probably won’t reach a point of having “herd immunity” without vaccines, because to get to that point the loss of life and disruption to our hospital systems and schools is beyond what we can accept as a society. Until then, we should all wear our masks! What can be more patriotic than putting the good of your family, your neighbors, and the country first in the time of crisis?